Exactly 100 years since the discovery of insulin by a team of Canadian researchers revolutionized the treatment of diabetes, the autoimmune disease continues to affect millions of Canadians with no cure in sight.
Advancements in science and technology have enabled us to monitor and manage diabetes better, but there is still room for improvement, experts say.
“Despite all of our advances, we still see a lot of complications of diabetes today, even in Canada, and so I think we have a lot of room to improve,” said Dr. Jeremy Gilbert, an endocrinologist at Sunnybrook Health Science Centre in Toronto.
More than 11 million Canadians, or one in three, are living with diabetes or prediabetes, according to Diabetes Canada.
Every hour of every day, at least 20 people are diagnosed with the disease and every 24 hours, more than 20 Canadians die of diabetes-related complications.
Diabetes is a chronic disease that occurs when the body is unable to produce or properly use insulin – a hormone that controls blood sugar levels.

If left uncontrolled, diabetes results in consistently high levels of blood sugar, which can lead to serious complications such as cardiovascular disease, vision loss, kidney failure, nerve damage and amputation.
Diabetes is also among the top 10 causes of death globally, according to the World Health Organization (WHO).
Since the 1921 discovery of insulin by Canadians Frederick Banting, Charles Herbert Best, James Bertram Collip and Britain’s John J.R. Macleod, insulin injections are still the most common and effective treatment for Type 1 diabetes.
However, the mode of delivery and monitoring have undergone upgrades.
Wearable glucose monitors and infusion pumps that deliver insulin continuously are considered a game-changer in managing diabetes, significantly improving the quality of life of patients.
Replacing the need to take urine or blood samples, a flash glucose metre can help detect sugar levels throughout the day by inserting a small sensor under the skin of a person’s upper arm or belly. The results are displayed on a reader and can be linked to a smartphone.
Gilbert said the glucose-sensing technologies that enable continuous real-time monitoring has been a “paradigm shift.”
“It’s a much more sophisticated way to monitor sugar levels,” said Dr. Michael Sefton, professor of biomedical engineering at the University of Toronto.
The hemoglobin A1c blood test, which allows patients and doctors to know how well the glucose has been controlled over the past three months, is another major achievement in diabetes research, according to Sefton.
“That gives a target that a person living with diabetes who is well-managed can shoot for.”
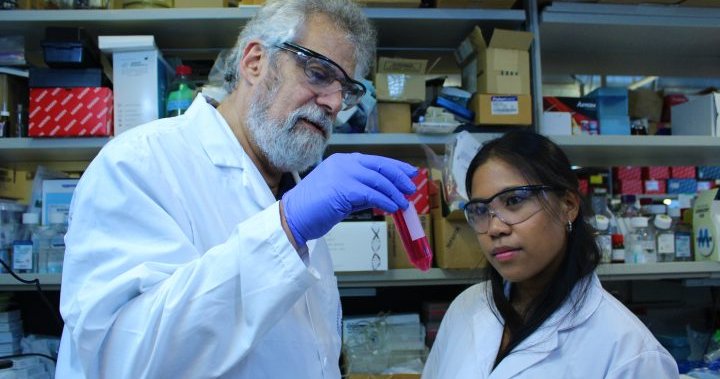
Dr. Michael Sefton and his team are researching a cell-based therapy to treat Type 1 diabetes.
Photo credit: Qin Dai U of T Engineering
There have also been advancements within insulin itself, which are safer to use and more user-friendly, said Gilbert.
The more common Type 2 diabetes, which accounts for more than 90 per cent of total diabetes cases, is becoming increasingly common in children in Canada.
A variety of oral medications can be taken to treat it. Lifestyle modifications, such as a healthy diet, exercise and weight loss can also help manage Type 2 diabetes.
New medications are available that reduce heart and kidney diseases beyond just the lowering of the sugar levels, said Gilbert.
“Many of the people who live with diabetes have already seen an improvement in their lifespan and improvement in their lifestyle over … the past 30 years,” said Sefton.
For the past decade, his lab at U of T’s Donnelly Centre for Cellular and Biomolecular Research has been working to develop a new way of treating diabetes to allow the transplant of pancreatic islets, the cells in a human pancreas that make insulin.
That work builds on a ground-breaking procedure by a research team at the University of Alberta. Termed the Edmonton Protocol and published in 2000, it involved pancreatic islets being isolated, purified and transplanted back from a donor into the livers of people living with Type 1 diabetes.
Now, Sefton’s team is focusing on transplanting the islets under the skin. They are collaborating with Dr. Tim Kieffer’s lab at the University of British Columbia in Vancouver. The project is funded by the non-profit Juvenile Diabetes Research Foundation (JDRF).
While still in the pre-clinical trial stage and being tested on small animals, Sefton believes this could change how diabetes is treated and become “quite routine” in the years to come.
“We think it’s the way of the future,” he said. “It’s a tough problem and so we want to take small, safe steps as we move forward.”

Another area that could prove pivotal is the use of stem cells for which several human clinical trials have been conducted.
Last month, Vertex Pharmaceuticals said Phase 1/2 clinical trials of a novel investigational stem cell-derived therapy for the treatment of Type 1 diabetes led to a 91 per cent reduction in daily insulin requirement and robust improvements in glucose control. The treatment was also generally well tolerated, the company said.
Going forward, the aim should be to find therapies that not only make people feel well, but are easy to take and do not result in significant side effects, said Gilbert.
Despite the progress, a cure still remains elusive and will be challenging to find, experts say.
“Most of our approaches now are just to manage the diabetes, but not necessarily cure it or put it into remission,” said Gilbert.
A cure remains a “tough goal” because there are still many unanswered questions about the disease and more research is needed, said Sefton.
Because there are several factors that contribute to the development of diabetes, it has been a challenge to cure it, said Gilbert.
But he remains hopeful.
“My hope is we continue to advance with the research we’re doing in Canada and worldwide to hopefully get to that cure sooner rather than later.”
© 2021 Global News, a division of Corus Entertainment Inc.







More Stories
B.C. to ban drug use in all public places in major overhaul of decriminalization | Globalnews.ca
Reduce salmonella in certain frozen chicken products: USDA to producers | CBC News
More than 115 cases of eye damage reported in Ontario after solar eclipse