The Current16:13‘Warmer’ transplant lungs stay viable longer, say scientists
When Rick Collins qualified for a double lung transplant, he was told that once a donor organ became available, he would have 90 minutes to get to the hospital.
But when that call did come, he didn’t have to rush.
“It was about 10 in the morning, [and] they said, ‘Could you come down at 4:30 p.m.?” said the 72-year-old from Clarington, Ont.
Collins said it already felt “surreal” to get the call he’d been waiting for, but when he and his wife Anne went to the hospital that afternoon, they were told the surgery would take place the next day.
“They said, OK … the lungs are coming in in the middle of the night, and we’re going to do it at 8 o’clock in the morning so that everyone gets here and is bright-eyed and bushy-tailed,” he told The Current’s Matt Galloway.

The change in timeline wasn’t the result of some kind of delay, but thanks to Collins’ participation in the trial of a new approach to lung transplants, pioneered by Canadian researchers.
Traditionally, once lungs are removed and marked for donation they’re kept on ice at between 0 and 4 C to slow degradation. That process offers roughly a six- to eight-hour window to get the organ into the chest of a waiting patient. A large proportion don’t make it in time.
Canadian scientists have been trialing a new method, which they say increases that window up to 36 hours by keeping the lungs at a warmer temperature during transit.
“We found out that if you keep organs at 10 degrees, that instead of shutting it down completely, some of the critical functions of cells … continue working,” said Dr. Shaf Keshavjee, a thoracic surgeon and chief of innovation at the University Health Network in Toronto.
Keshavjee said there’s been evidence to support keeping donated lungs at a warmer temperature for some time, but there was no practical way to achieve it.
“What we’ve designed is a cooler pack that actually has a chemical in it that goes from liquid to solid at 10 degrees … it keeps the organ at 10 degrees exactly, for 36 hours,” he said.
“Basically we can pick up a lung anywhere in North America, bring it back and transplant it.”

Keshavjee and his team hope to publish the results of their study soon. The researchers also hope that the increased window might ultimately mean fewer organs go to waste, and Keshavjee said the concept could potentially be applied to other organs.
According to the most recent figures available from the Canadian Institute for Health Information, 352 people received a lung transplant in Canada in 2021. As of Dec. 31 that year, 222 people were still waiting for a lung transplant, and 37 people had died on the wait-list in the 12 months previous.
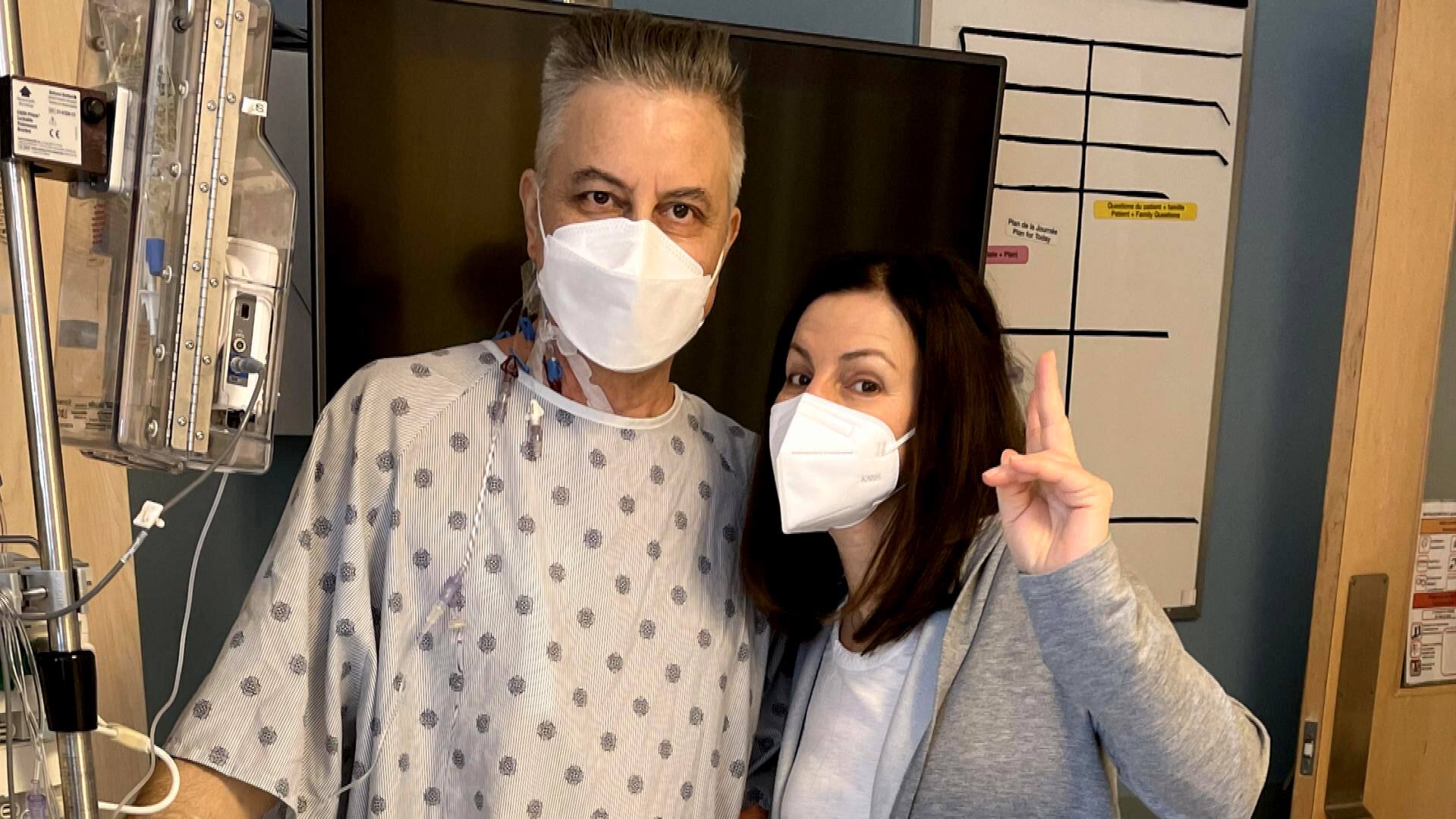
Collins found recovery ‘miraculous’
Collins underwent the double lung transplant in Toronto in late 2021. He was part of a trial of 70 patients who underwent this method.
Prior to transplant he had relied on oxygen tanks to cope with the deteriorating effects of alpha-1 antitrypsin, an inherited disorder that left him with about 15 per cent lung capacity. Everyday chores like taking out the garbage had become impossible, and even holding a conversation was difficult.
“I might be a little halting … [I] might have to catch a breath and then finish the sentence,” said Collins.
Most people don’t think about live organ donation until it hits close to home. That’s exactly what happened to CBC’s Ioanna Roumeliotis when her brother suddenly needed a kidney transplant. She tells her family’s story of what it’s like to give and to receive a life-saving organ.
Collins had expected to spend three weeks in hospital after the operation, but was out in nine days — a recovery he describes as “miraculous.”
“I thought I was Superman to begin with,” he joked. “But then once you get into the 10-degree thing … that’s got to have a lot to do with it.”
He said the transplant has been “life-changing,” and he’s back to “doing just about everything I used to do … just trying to catch up on some stamina.”
He and his wife Anne have just celebrated their 50th wedding anniversary. They even shared a dance, something that has not been possible for about 10 years, he told The Current.
Keshavjee said he’s grateful for the patients who have participated in the trial.
“It’s been an amazing journey in terms of being able to deliver like that for patients like Rick, where they’re facing a life-threatening condition,” Keshavjee said.
Toronto’s University Health Network says it has completed the first double lung transplant where lungs were delivered by drone.
Transplant can be planned, not rushed
Keshavjee said one of the major benefits of increasing the viability window for donated lungs is that it makes transplants a “schedule-able operation.”
Previously, transplants would happen when an organ became available, often at short notice, prompting the cancellation of other non-emergency scheduled surgeries.
With 36 hours, “you don’t have to rush into it in the middle of the night,” he said, adding that it also creates more flexibility for patients.
“Canada is a big country, so patients can now wait at home, further away … they don’t have to move to within one hour of Toronto like we used to do historically,” he said.
“For patients facing end-stage lung disease, that’s a huge improvement in quality of life to be close to family and friends.”
Keshavjee said the patients involved in the trial have been surprised at these changes.
“It just happens. They got their lung transplant and they’re off back to their life,” he said. “It’s absolutely fantastic and so rewarding to see that.”






More Stories
Global measles cases nearly doubled in one year, researchers say
How to make conversations with aging parents a little less awkward | CBC Radio
N.S. mom calls for better ultrasound access after private clinic reveals twins | Globalnews.ca